CGM for Non-Diabetics: Hype, Health, or Something In Between?

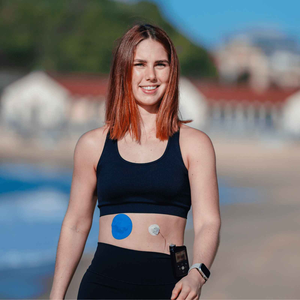
You might have noticed continuous glucose monitors appearing in wellness spaces that once had nothing to do with diabetes. Influencers talk about glucose spikes. Apps promise personalised insights. Friends without diabetes mention wearing a sensor for a month to understand their body better.
If you use a CGM for medical reasons, or care for someone who does, this trend can feel confusing or even frustrating. You might wonder whether CGM for non diabetics is genuinely useful, overhyped, or missing important context. We are going to slow this down and look at what the science actually says, where CGM for non diabetics may help, and where expectations need to be realistic.
Why CGM for non diabetics is gaining attention
CGM for non diabetics sits at the intersection of biohacking, preventive health, and data driven wellness. Many people are looking for ways to feel more in control of energy, weight, mood, and long term health. CGM for non diabetics promises a window into how food, stress, sleep, and movement affect the body in real time.
This mirrors what many CGM users already know from lived experience. Our article on how food affects your blood glucose levels according to your CGM shows that context matters as much as the number itself.
What CGM data actually shows in people without diabetes
CGM for non diabetics measures interstitial glucose, just as it does for people with diabetes. In people without diabetes, glucose levels usually stay within a narrow range, with small rises after eating and gradual returns to baseline.
Without guidance, CGM for non diabetics can make normal responses feel like problems. This is similar to what new CGM users experience, which is why your first Freestyle Libre sensor focuses so heavily on expectation setting rather than numbers alone.
Potential benefits of CGM for non diabetics
Used thoughtfully, CGM's for non diabetics can offer learning rather than optimisation.

Awareness of daily patterns
CGM's for non diabetics can highlight how skipped meals, poor sleep, or dehydration affect glucose stability. Our guide on dehydration and diabetes shows how hydration alone can influence readings.
Behaviour change through feedback
Short term use of CGM's for non diabetics may encourage balanced meals and gentle movement, such as walking after eating, without chasing perfect graphs.
Where CGM for non diabetics can fall short
Normal glucose rises are not harmful
Glucose increases after meals are expected. CGM's for non diabetics can unintentionally promote food fear if normal spikes are framed as damage.
Data without education can increase anxiety
We see this even in long term CGM users, which is why articles like burnt out from managing your diabetes resonate so strongly.
Sensor accuracy and wear issues matter
Compression lows, sweat, and adhesion problems can all distort readings. These challenges are covered in top CGM patch issues and how to fix them.
CGM for non diabetics versus medical CGM use
|
Aspect |
CGM for non diabetics |
CGM for diabetes |
|
Purpose |
Awareness and learning |
Medical management |
|
Duration |
Short term use |
Ongoing |
|
Interpretation |
Often self guided |
Clinically informed |
|
Risk of over interpretation |
Higher |
Lower with education |
This distinction matters, especially for people who rely on CGM's for safety and daily decisions.
How this trend affects people who rely on CGMs
When CGM's for non diabetics are marketed as a wellness upgrade, it can unintentionally downplay the realities of living with a CGM long term. Skin reactions, sensor failures, and wear time are not abstract issues.

Resources like how long should a CGM patch last and why your CGM sensor needs extra protection in summer exist because wearability directly affects quality of life. Supportive tools such as CGM patches and adhesive wipes are not about performance optimisation. They are about comfort, consistency, and confidence.
A grounded way to think about CGM's for non diabetics
CGM use for non diabetics sits somewhere between curiosity and care. It can support learning when used with context and self compassion. Without that, it risks turning normal biology into a problem to fix.
At Type Strong, we believe CGM technology should support you, not pressure you. Whether CGM for non diabetics remains a trend or not, the goal stays the same - helping people live with confidence, not constant correction.
References
Ajana, S. et al., 2020. Continuous glucose monitoring in people without diabetes - a systematic review. Journal of Diabetes Science and Technology.
https://journals.sagepub.com/doi/10.1177/1932296820958756
Hall, H. et al., 2019. Postprandial glucose responses in healthy adults. American Journal of Clinical Nutrition.
https://academic.oup.com/ajcn/article/110/3/590/5512015
Zeevi, D. et al., 2015. Personalised nutrition by prediction of glycaemic responses. Cell.