If you live with Type 1 diabetes, you’ll know that research news is constant – new diets, devices, or drugs that could make management easier. Most of these stories fade, but every now and then one makes headlines for good reason. Lately, scientists have been looking closely at baricitinib, a medication originally designed for arthritis.
The question researchers are asking is simple but powerful: could a drug already on the shelf help people with Type 1 diabetes keep making some of their own insulin for longer?
Disclaimer: This article is for education only. It is not medical advice. Always speak to your healthcare team before starting or changing any treatment.
What is baricitinib and why are scientists studying it?
Baricitinib is a Janus kinase (JAK) inhibitor. In arthritis, it helps reduce joint inflammation by calming the immune system. Since Type 1 diabetes is an autoimmune condition, researchers wondered if the same approach might work to protect insulin-producing beta cells in the pancreas.
The logic is clear: if the immune system is attacking those cells, perhaps slowing the attack with a drug like baricitinib could preserve insulin production, at least for a while. For people newly diagnosed, that could mean more stable blood sugars and fewer sharp swings.
What do recent baricitinib trials in Type 1 diabetes show?
The latest trial, published in The Lancet (Rigby et al., 2023), tested baricitinib in people who had just been diagnosed with Type 1 diabetes. Some of the key findings were:
- Beta cells held on for longer – people taking baricitinib had higher C-peptide levels, showing their pancreas was still making insulin.
- Insulin doses were lower – the treatment group generally needed less injected insulin to stay in range.
- HbA1c improved slightly – though the changes weren’t dramatic, they were better than in the placebo group.
- Side effects matched what’s seen in arthritis use – mild infections and small changes in blood tests.
This doesn’t mean baricitinib is a cure, but it does hint at a new way forward: slowing, not stopping, the loss of insulin production in early Type 1.
Trial results for baricitinib in new-onset Type 1 diabetes
|
Outcome |
Baricitinib group |
Placebo group |
|
Beta cell function (C-peptide) |
Preserved at 1 year |
Declined faster |
|
Insulin dose needed |
Slightly lower |
Higher |
|
HbA1c |
Small improvement |
Minimal change |
|
Common side effects |
Mild infections, lab changes |
Few issues |
(Rigby et al., 2023, The Lancet)
Is baricitinib safe for long-term use?
That’s the part we don’t know yet. In arthritis, people can stay on baricitinib for years, but doctors carefully monitor them for risks like infections, blood clots, or liver problems. In Type 1 diabetes, the evidence only covers the first year of use.

Researchers are clear: baricitinib is not a cure. It might buy some time by protecting beta cells in those early months after diagnosis, but we don’t yet know how safe or effective it would be if used for decades. Larger and longer studies are already underway.
What does this mean for your diabetes care right now?
Hearing about new treatments is always exciting, but they are still years from being part of everyday care. Right now, the tools that matter most are the ones you use daily – insulin, your CGM, and the routines that keep them reliable.
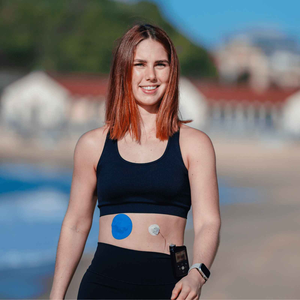
And that reliability often comes down to the simple things: making sure your sensor stays put. If your patch starts peeling, your CGM can lose accuracy. That’s why many people use CGM patches or adhesive wipes to keep sensors secure. For active users, Dexcom G7 patches and Omnipod patches are designed to last through workouts, swimming, and long days.
People also ask
Can arthritis medication help diabetes?
Some arthritis drugs like baricitinib are being trialled in Type 1 diabetes. Early results are encouraging, but they are not approved treatments yet.
What new treatments are being tested for Type 1 diabetes?
Research includes immune therapies like teplizumab, stem-cell-derived beta cells, and more advanced closed-loop insulin systems.
Why is beta cell preservation important?
Even small amounts of natural insulin help smooth out glucose swings and reduce long-term complications.
How can I support my care today?
Focus on steady CGM use, good skin prep, balanced meals, and open conversations with your diabetes team.
Related reading
- 5 best CGMs in 2025
- How long should a CGM patch last
- Why your CGM sensor needs extra protection in summer
What this means for people with Type 1 diabetes
The research into baricitinib shows that scientists are working hard to expand treatment options for Type 1 diabetes. But it’s still experimental and not part of daily care. What you can count on today is the combination of insulin, your CGM, and the tools that keep it reliable – like patches and adhesive wipes that help your sensor stay in place. These supports make sure you get accurate readings and the confidence to manage food, insulin, and activity each day.

The road forward for Type 1 diabetes treatment
Baricitinib highlights the potential of repurposed drugs to shape the future of diabetes care, but more study is needed before it becomes standard. For now, the strongest path is built on what we already know works: insulin, CGM technology, and the practical products that keep them steady. With secure patches and good skin preparation, your CGM can deliver the consistent insights you need today, while research continues toward tomorrow’s breakthroughs.
References
Rigby, M.R., et al. (2023). Baricitinib in new-onset type 1 diabetes: a randomised, double-blind, placebo-controlled trial. The Lancet, 401(10389), pp.1091-1102. Available at: https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(23)00265-0
National Institutes of Health (NIH). (2022). Baricitinib: Drug information. MedlinePlus. Available at: https://medlineplus.gov/druginfo/meds/a617007.html
Diabetes UK. (2023). New treatments for type 1 diabetes. Available at: https://www.diabetes.org.uk/research/research-round-up/type-1